Biden’s Initiative for Medicare and Medicaid to Cover Expensive Weight-Loss Medications Like Wegovy
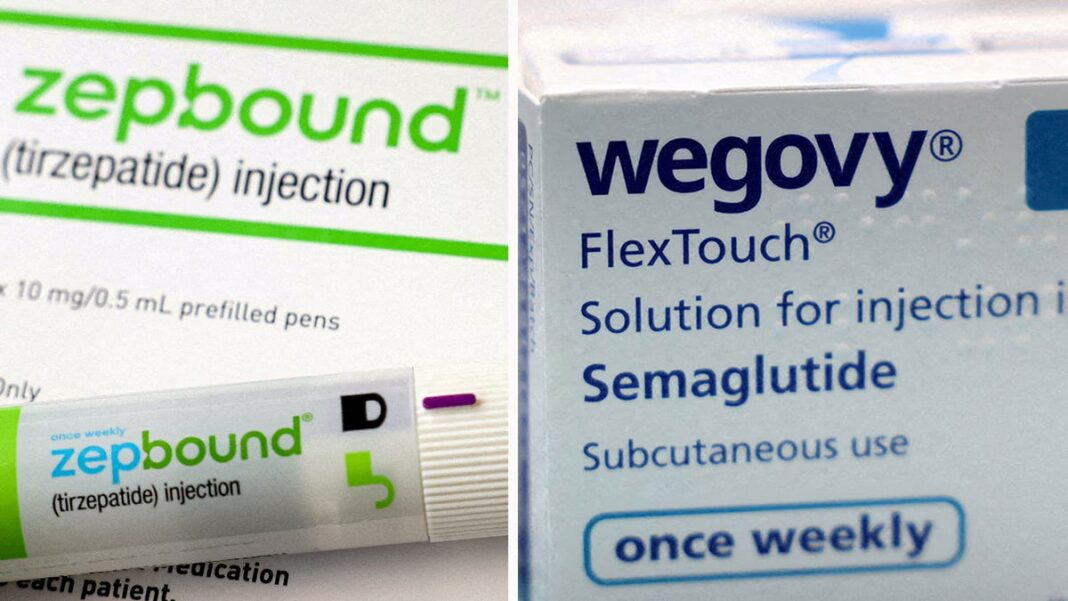
On Tuesday, the Biden administration revealed its intention to include coverage for a new category of high-priced anti-obesity medications, such as Wegovy and Zepbound, for individuals enrolled in Medicare and Medicaid.
Typically, Medicare—the health program for older adults—has been legally barred from covering weight-loss drugs for seniors who are obese but lack diabetes or heart disease.
The Department of Health and Human Services has proposed a rule that suggests roughly 3.4 million Medicare recipients may qualify for these medications, which can exceed $1,000 monthly. While some states currently allow Medicaid to pay for obesity drugs, most do not. This new proposal could potentially make around 4 million Medicaid beneficiaries eligible for coverage.
Many Americans have found it difficult to afford these popular weight-loss medications known as GLP-1, or glucagon-like peptide-1 receptor agonists. Originally developed for diabetes treatment, newer variants like Wegovy and Zepbound are now authorized for use in individuals with obesity.
Dr. Fatima Cody Stanford, an obesity medicine expert at Massachusetts General Hospital and Harvard Medical School, praised the move, saying, “This is a significant positive advancement by the White House and CMS to ensure that those enrolled in Medicaid and Medicare, who often bear the most severe impacts of obesity, gain access to anti-obesity medications.”
These medications come with high price tags. For instance, Wegovy from Novo Nordisk is priced at approximately $1,349 each month. In comparison, the same drug is sold for $186 in Denmark, $140 in Germany, and $92 in the UK, as highlighted during a hearing of the Senate Committee on Health, Education, Labor, and Pensions in September.
During that September session, Senators interrogated Novo Nordisk’s CEO regarding the substantial price differences for Wegovy and other diabetes medications like Ozempic in the U.S. compared to Europe.
Diabetes drugs such as Ozempic are frequently covered by employers providing health insurance and private insurance plans.
Both Ozempic and Wegovy, produced by Novo Nordisk, share a common active ingredient called semaglutide, though Wegovy is prescribed in higher doses. Meanwhile, Zepbound and the diabetes treatment Mounjaro, manufactured by Eli Lilly, utilize a different compound, tirzepatide, which enhances weight-loss effectiveness through dual action.
A recent survey conducted by Mercer, a benefits consulting firm, revealed that 44% of large employers now provide coverage for GLP-1 drugs for obesity, an uptick from 41% in the previous year.
Officials from the Biden administration did not provide immediate details regarding the financial implications for taxpayers resulting from the extension of weight-loss medication coverage. However, they indicated that this inclusion could reduce out-of-pocket costs for Medicare recipients by up to 95%.
Earlier this year, North Carolina’s health program for state employees stopped covering prescription weight-loss medications like Wegovy and Saxenda owing to their steep costs.